Save a Tooth, Maybe Save a Life
By David Landwehr, D.D.S., M.S.
“Your natural teeth are worth saving. See an endodontist today.” So reads the banner headline on the front page of the AAE website. As a practicing endodontist for more than 20 years I couldn’t agree more and I am pleased to have helped patients retain thousands of teeth over my career. However, I am more proud of the lives I have impacted by recognizing when a presenting pathology was not of endodontic origin. It is not uncommon to get a note of thanks from a patient expressing gratitude for relieving their pain or seeing them on an emergency basis, but my favorite notes arrive annually from the same patient. The card arrives with the same inscription: “This is our anniversary, thanks again for saving my life.” This patient presented with a necrotic tooth, but also had a salivary gland tumor that had nothing to do with her dental issues. Because I was able to identify her needs as a patient over and above her endodontic needs, she was immediately referred for biopsy and appropriate treatment was initiated resulting in the most favorable outcome- a long-term cure.
The use of pulp testing in conjunction with medical history, dental history, clinical examination and radiographic findings has been my standard routine to differentiate pulpal pathology from that of a non-inflammatory or non-dental etiology. However, given the diagnostic limitations of pulp testing, I find myself potentially placing an undue amount of importance on radiographic findings, especially with the emergence of CBCT. Periapical cysts and periapical granulomas make up the majority of radiographic lesions in the tooth bearing regions of the jaws.1,2 According to a 2012 systematic review of cross-sectional studies evaluating the periapical status of over 300,000 teeth, 5% of all teeth had periapical radiolucencies.3 The prevalence of periapical radiolucencies in the population illustrates the critical importance of being able to formulate an accurate differential diagnosis of these radiographic abnormalities. Many of these radiolucencies are asymptomatic and discovered on routine radiographs by my referring partners. As an endodontist, it is easy to assume that any periapical radiolucency associated with pain is of pulpal or inflammatory origin, especially if the tooth has a significant restorative history or a previous history of pulpitis symptoms. However, as a pathologist I am constantly reminded that numerous disease entities of variable clinical significance can be identified in the periradicular regions and differentiating the typical endodontic presentation from that of a potentially more life threatening or insidious etiology is necessary to ensure ideal management and outcome.
In many cases, the radiographic findings associated with non-inflammatory pathologies can very closely mimic the presentation of the more common periapical cyst or periapical granuloma and there is no way to definitively determine the clinical importance of a lesion based on radiographic features alone. However, accurate radiographic interpretation of the bone and dental abnormalities in conjunction with a thorough review of the medical history, dental history, pulp testing and clinical examination will allow me to systematically formulate a differential diagnosis.
I first determine if the radiographic presentation is unilocular or multilocular. Periapical cysts and periapical granulomas have a wide spectrum of radiographic presentations with some causing extensive bone destruction and others resulting in minimal radiographic change. Irrespective of size, the presentation of periapical inflammatory disease should be radiographically unilocular and confirmed with a lack or responsiveness to pulp testing. If a multilocular radiolucency is identified on a periapical image, I will obtain a CBCT to confirm the multilocular growth pattern and extent of the lesion and a biopsy will most likely be recommended. The differential diagnosis of multilocular radiolucencies is extensive, but the most common are odontogenic keratocyst, ameloblastoma, and central giant cell lesion.
Although a multilocular radiolucency is consistent with a non-inflammatory etiology, any of the previously mentioned multilocular radiolucencies can also present as a unilocular lesion in its earlier stages prior to reaching full growth potential. As a result, other radiographic features need to be considered when forming a differential diagnosis. In my experience, endodontic lesions of inflammatory origin present as radiolucent lesions with no indication of radiopacity. As a result, if I identify any evidence of radiopacity, my suspicion of a non-inflammatory etiology will be elevated, especially if a limited restorative history is present or pulp testing is inconclusive. Exceptions to this rule would include condensing osteitis and maxillary sinusitis of endodontic origin.
I don’t often encounter asymptomatic radiolucencies resulting from simultaneous pulpal necrosis in multiple teeth, but I can’t rule out the possibility on radiographic examination alone. Pulp testing and dental history are important if multiple necrotic pulps are suspected, but a multifocal presentation also raises my concern about a non-bacterial etiology. Periapical cemento-osseous dysplasia (PCOD) is the most common multifocal radiolucency to mimic lesions of endodontic origin and has been known by a variety of terms in the literature. Like the other benign fibro-osseous lesions, PCOD is characterized by the replacement of bone with fibrous and mineralized tissue. The radiographic presentation can be highly variable. Some cases are almost purely radiolucent with minimal radiopaque flecks while more advanced lesions may be mostly radiopaque. Typically I will make the diagnosis of PCOD based on clinical presentation, pulp testing and radiographic findings and no treatment is indicated. However, if there is uncertainty about the diagnosis a biopsy can be obtained, but this comes with an increased risk for infection, bone necrosis or a disruption in the pulpal blood supply.
Peripheral demarcation of the radiolucency is critical to me and this may seem counterintuitive because periapical cysts and periapical granulomas are the most common ill-defined and well-defined radiolucencies. However, I closely consider the outline of any radiolucency because the differential diagnosis for ill-defined radiolucencies is more ominous. Rapid cortical expansion or perforation of the cortical plate, extensive tooth mobility, irregular root resorption and a “moth eaten” appearance suggest malignancies should be included in the differential diagnosis (Figures 1-3). If the results of the pulp testing are not confirmed by the clinical findings at the time of root canal treatment and the radiographic lesion is ill-defined, further investigation and referral may be indicated.
Most radiographic abnormalities encountered on a daily basis in the endodontic setting will be due to a bacterial cause as the result of a necrotic pulp. However, when I encounter an atypical presentation and the pieces of the diagnostic puzzle don’t fit I will also begin to consider the potential for a developmental, metabolic or neoplastic etiology that may closely resemble an inflammatory cause. A multilocular radiolucency should not be the result of a necrotic pulp and further diagnostic workup is indicated when this type of change is identified. Most radiographic lesions of inflammatory origin are going to be radiolucent and the presence of calcification suggests a higher likelihood for a non-pulpal etiology. Furthermore, a multifocal presentation should arouse suspicion about non-inflammatory etiologies, especially if the dental history and pulp testing are not consistent with pulp necrosis in multiple teeth. Periapical inflammatory disease can be well-defined and corticated radiographically or the lesion can have ill-defined margins when the radiographic change is confined to the medullary spaces. If a lesion is ill-defined I want to be absolutely certain the clinical findings at the time of treatment corroborate the pulp testing results, especially if there are any signs of aggressive behavior radiographically.
This has been a very brief overview of the radiographic features I consider in making a systematic differential diagnosis of periapical lesions. Consistently looking at radiographic abnormalities and asking the same series of questions has enabled me to critically evaluate and differentiate lesions of endodontic origin from pathologies not related to an inflammatory cause. This is our responsibility as endodontists: save as many teeth as possible, but recognize and appropriately refer when we encounter pathologies unrelated to the dental pulp. Endodontics is about more than saving teeth.
Figure 1
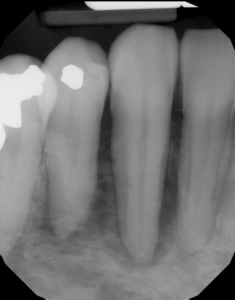
52 year-old female with a chief complaint of “pressure sensitivity for six months and teeth feel loose.”
Medical history: gastric bypass, mild hypertension controlled with meds
Dental history: Symptoms started in 27/28 area, but now extend past midline into 22/23 area.
Examination does not demonstrate any expansion of cortical plates and there is no swelling or mobility of teeth. However, the bone in mandibular anterior region feels slightly spongy on palpation. Mandibular teeth (22- 30) respond to cold testing and are asymptomatic to percussion. Mucosal lining and gingival tissues are within normal limits with no evidence of ulceration.
Figure 2
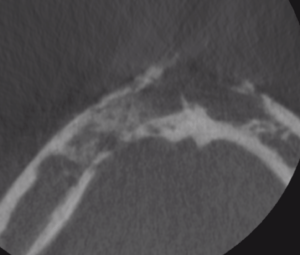
Axial view of a small field cone beam CT demonstrates large, irregular shaped, ill-defined (moth eaten pattern) low-density area associated with the anterior mandibular area extending from the right premolar region to the left premolar region. The buccal and lingual cortical plates are perforated without any signs of bone expansion, or periosteal reaction. A generalized widening of the PDL spaces and loss of lamina dura associated with the premolars and canines was also noted in the sections containing teeth.
Figure 3

A volumetric rendering demonstrates a “moth-eaten” pattern of bone loss and significant bone destruction. This aggressive clinical presentation suggested malignancy and biopsy confirmed a Non-Hodgkin Lymphoma.
References:
- Koivisto T, Bowles WR, Rohrer M: Frequency and distribution of radiolucent jaw lesions: a retrospective analysis of 9,723 cases. J Endod 38:729, 2012.
- Becconsall-Ryan K, Tong D, Love RM: Radiolucent inflammatory jaw lesions: a twenty-year analysis. Int Endod J 43:859, 2010.
- Pak JG, Fayazi S, Shane N et al: Prevalence of periapical radiolucency and root canal treatment: a systematic review of cross-sectional studies. J Endod 38:1170, 2012.




