Retreatment of Bioceramic Sealer-Obturated Canals

By Dr. Jianing (Jenny) He
Calcium silicate-based bioceramic sealers have been growing in popularity in the last 15 years. According to a recent survey, 49% of the AAE members and 27% of the ADA members reported using bioceramic sealers, which have surpassed resin-based sealers and become the most widely-used sealer type among endodontists 1. While many clinicians are attracted to the efficiency and simplicity of the bioceramic sealer-based single-cone technique, the wider acceptance of bioceramic sealers is also driven by the growing body of evidence demonstrating their favorable properties and clinical effectiveness. The reported success rates of cases obturated with bioceramic sealer-based single-cone technique range between 90 and 99% with no significant differences noted between this technique and warm vertical compaction technique using resin sealers 2-6.
Despite the high success rates reported in the literature, treatment failure inevitably occurs necessitating the need for retreament. Retreatability of bioceramic sealers is a perceived concern expressed by many clinicians because the materials are hard-setting and are not soluble in traditional solvents such as chloroform7. In vitro studies on the retreatability of these materials show inconsistencies and results seem to depend on the canal anatomy, whether gutta-percha is placed to length during the initial treatment, and whether a solvent is used. When gutta-percha is placed to length during the initial treatment, re-establishing working length and patency is possible in most cases especially in large, straight canals, and when chloroform is used 8-10. However, if there is a significant amount of set sealer present in the apical portion of a canal, it can be difficult to get through this blockage to achieve patency using traditional retreatment techniques (Figure 1) 9.
Efforts have been made to develop supplemental protocols to facilitate the removal of set bioceramic sealers. These protocols include the use of alternative solvents, mechanical removal, and the use of active irrigation. Various acids such as formic acid, hydrochloric acid, acetic acid, and citric acid have been tested on bioceramic sealers with mostly negative results 11,12. Although hydrochloric acid was reported to reduce the time needed to achieve patency, the difference is not clinically significant and its use is limited due to its highly corrosive nature 13. Citric acid has shown potential to cause surface changes and mass loss in certain bioceramic sealers which may facilitate their removal 14. However, an effective and clinically useful solvent for bioceramic sealers is not yet available. Therefore, mechanical means are necessary to remove the set sealer.
One of the mechanical means is the use of ultrasonic instruments activated directly on the set sealer, which is effective in breaking up the material when it is visible and accessible. Clinical anecdotes also show that a stiff hand file such as C or C+ file can be used to penetrate the set sealer. In addition, mechanical enlargement of the canal space two sizes greater than the initial size has been shown to minimize the amount of residual sealer 15. However, additional dentin removed during this process may compromise the mechanical strength of the tooth.
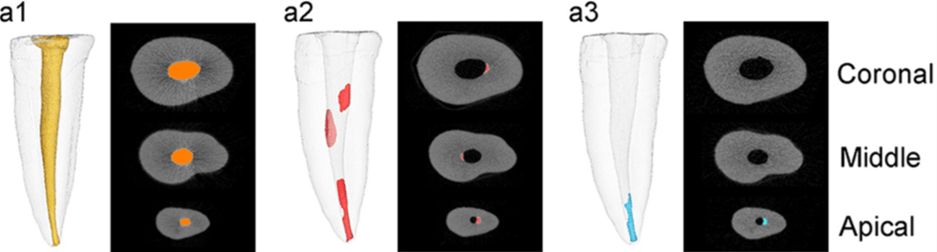
Hydrodynamic forces generated by sonic, ultrasonic, or laser energy in active irrigation can disrupt and remove tissue debris, biofilms, as well as root filling materials including bioceramic sealers without the removal of dentin. Among the various active irrigation systems, ultrasonic activated and laser assisted irrigation with Photon-Induced Photoacoustic Streaming (PIPS) and Shock Wave Enhanced Emission Photoacoustic Streaming (SWEEPS) modes appear to be useful in removing additional bioceramic sealers (Figure 2) 16-21. XP-3D Finisher used with irrigants has shown similar or better efficacy as ultrasonic activation in sealer removal, though no system has proven superiority.
One consistent finding reported in all published studies on retreatment is that no root filling material can be completely removed despite the use of supplemental protocols regardless of the sealer type. It is particularly difficult to remove filling material from canal irregularities such as the isthmus, lateral canals, and deep in the dentin tubules 22. Although the impact of residual sealer on the success of retreatment has not been studied, it is unlikely that it will significantly compromise the treatment outcome if the primary etiology of the initial treatment failure has been addressed, which is the most important goal during retreatment. Locating and treating previously missed canals, correcting previous procedural errors and re-establishing working length are essential to the success of retreatment. Complete removal of existing root filling materials including the sealer is desirable to achieve thorough disinfection of the root canal space but not always possible. The selection of a sealer used in root canal obturation should be based on whether it possesses the properties to fulfil the functions of a sealer to optimize the chance of treatment success. Sealing ability, biocompatibility, dimensional stability, and antibacterial properties are more important considerations over retreatability.
In summary, concerns over the retreatability of bioceramic sealers do not seem to be substantiated by scientific or empirical evidence. Retreatment of canals obturated with bioceramic sealers is possible in most cases using traditional tools and techniques. Supplemental mechanical removal and active irrigation using ultrasonics, XP-Finisher and lasers help to maximize material removal.
Figure 1: SEM image showing an apical plug of set bioceramic sealer.
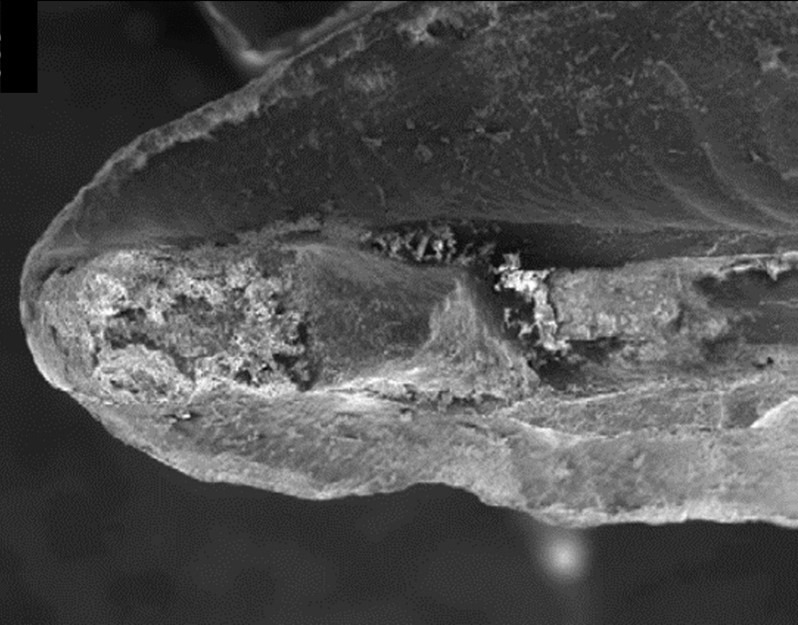
Figure 2: Reconstructed micro-CT images showing effective removal of bioceramic sealer with PIPS. a1, after obturation; a2, after mechanical retreatment; a3, after PIPS-assisted irrigation. (Yang et al., BMC Oral Health (2021) 21:275)
References:
- Swiss, R. (2022). Current Trends in Endodontic Obturation: A Web Based Survey Comparing ADA and AAE Members. MS (UNIFORMED SERVICES UNIVERSITY OF THE HEALTH SCIENCES, POSTGRADUATE DENTAL COLLEGE).
- Chybowski, E.A., Glickman, G.N., Patel, Y., Fleury, A., Solomon, E., and He, J. (2018). Clinical Outcome of Non-Surgical Root Canal Treatment Using a Single-cone Technique with Endosequence Bioceramic Sealer: A Retrospective Analysis. J Endod 44, 941-945. 10.1016/j.joen.2018.02.019.
- Pontoriero, D.I.K., Ferrari Cagidiaco, E., Maccagnola, V., Manfredini, D., and Ferrari, M. (2023). Outcomes of Endodontic-Treated Teeth Obturated with Bioceramic Sealers in Combination with Warm Gutta-Percha Obturation Techniques: A Prospective Clinical Study. J Clin Med 12. 10.3390/jcm12082867.
- Walsh, R.M., Attar, S., Turner, C.L., Pistocchi, R., Allen, L., and Woodmansey, K.F. (2023). Clinical outcomes of non-surgical root canal obturations using NeoMTA: A retrospective series of case reports. Aust Endod J 49 Suppl 1, 455-461. 10.1111/aej.12712.
- Zavattini, A., Knight, A., Foschi, F., and Mannocci, F. (2020). Outcome of Root Canal Treatments Using a New Calcium Silicate Root Canal Sealer: A Non-Randomized Clinical Trial. J Clin Med 9. 10.3390/jcm9030782.
- Kim, J.H., Cho, S.Y., Choi, Y., Kim, D.H., Shin, S.J., and Jung, I.Y. (2022). Clinical Efficacy of Sealer-based Obturation Using Calcium Silicate Sealers: A Randomized Clinical Trial. J Endod 48, 144-151. 10.1016/j.joen.2021.11.011.
- Guivarc’h, M., Jeanneau, C., Giraud, T., Pommel, L., About, I., Azim, A.A., and Bukiet, F. (2020). An international survey on the use of calcium silicate-based sealers in non-surgical endodontic treatment. Clin Oral Investig 24, 417-424. 10.1007/s00784-019-02920-1.
- Agrafioti, A., Koursoumis, A.D., and Kontakiotis, E.G. (2015). Re-establishing apical patency after obturation with Gutta-percha and two novel calcium silicate-based sealers. Eur J Dent 9, 457-461. 10.4103/1305-7456.172625.
- Hess, D., Solomon, E., Spears, R., and He, J. (2011). Retreatability of a bioceramic root canal sealing material. J Endod 37, 1547-1549. 10.1016/j.joen.2011.08.016.
- Oltra, E., Cox, T.C., LaCourse, M.R., Johnson, J.D., and Paranjpe, A. (2017). Retreatability of two endodontic sealers, EndoSequence BC Sealer and AH Plus: a micro-computed tomographic comparison. Restor Dent Endod 42, 19-26. 10.5395/rde.2017.42.1.19.
- Carrillo, C.A., Kirkpatrick, T., Freeman, K., Makins, S.R., Aldabbagh, M., and Jeong, J.W. (2022). Retrievability of Calcium Silicate-based Root Canal Sealers During Retreatment: An Ex Vivo Study. J Endod 48, 781-786. 10.1016/j.joen.2022.02.009.
- Garrib, M., and Camilleri, J. (2020). Retreatment efficacy of hydraulic calcium silicate sealers used in single cone obturation. J Dent 98, 103370. 10.1016/j.jdent.2020.103370.
- Rezaei, G., Liu, X., and Jalali, P. (2023). Efficacy of Different Solvents for Achieving Patency in Teeth Obturated Using Bioceramic Sealer. J Endod 49, 219-223. 10.1016/j.joen.2022.12.001.
- Drukteinis, S., Bilvinaite, G., and Sakirzanovas, S. (2024). The Impact of Citric Acid Solution on Hydraulic Calcium Silicate-Based Sealers and Root Dentin: A Preliminary Assessment. Materials (Basel) 17. 10.3390/ma17061351.
- Roggendorf, M.J., Legner, M., Ebert, J., Fillery, E., Frankenberger, R., and Friedman, S. (2010). Micro-CT evaluation of residual material in canals filled with Activ GP or GuttaFlow following removal with NiTi instruments. Int Endod J 43, 200-209. 10.1111/j.1365-2591.2009.01659.x.
- Crozeta, B.M., Lopes, F.C., Menezes Silva, R., Silva-Sousa, Y.T.C., Moretti, L.F., and Sousa-Neto, M.D. (2021). Retreatability of BC Sealer and AH Plus root canal sealers using new supplementary instrumentation protocol during non-surgical endodontic retreatment. Clin Oral Investig 25, 891-899. 10.1007/s00784-020-03376-4.
- Farrayeh, A., Akil, S., Eid, A., Macaluso, V., Mancino, D., Haikel, Y., and Kharouf, N. (2023). Effectiveness of Two Endodontic Instruments in Calcium Silicate-Based Sealer Retreatment. Bioengineering (Basel) 10. 10.3390/bioengineering10030362.
- Hassan, R., and Elzahar, S. (2022). Cleaning Efficiency of XP Finisher, XP Finisher R and Passive Ultrasonic Irrigation Following Retreatment of Teeth Obturated with TotalFill HiFlow Bioceramic Sealer. Eur Endod J 7, 143-149. 10.14744/eej.2022.39358.
- Suk, M., Bago, I., Katic, M., Snjaric, D., Munitic, M.S., and Anic, I. (2017). The efficacy of photon-initiated photoacoustic streaming in the removal of calcium silicate-based filling remnants from the root canal after rotary retreatment. Lasers Med Sci 32, 2055-2062. 10.1007/s10103-017-2325-4.
- Volponi, A., Pelegrine, R.A., Kato, A.S., Stringheta, C.P., Lopes, R.T., Silva, A.S.S., and Bueno, C. (2020). Micro-computed Tomographic Assessment of Supplementary Cleaning Techniques for Removing Bioceramic Sealer and Gutta-percha in Oval Canals. J Endod 46, 1901-1906. 10.1016/j.joen.2020.09.010.
- Yang, R., Han, Y., Liu, Z., Xu, Z., Liu, H., and Wei, X. (2021). Comparison of the efficacy of laser-activated and ultrasonic-activated techniques for the removal of tricalcium silicate-based sealers and gutta-percha in root canal retreatment: a microtomography and scanning electron microscopy study. BMC Oral Health 21, 275. 10.1186/s12903-021-01638-5.
- Uysal, B.A., and Arican, B. (2024). Comparison of the dentin tubule penetration of AH Plus, WellRoot ST, and MTA BioSeal after obturation, retreatment, and re-shaping of the root canals. Microsc Res Tech 87, 114-121. 10.1002/jemt.24416.




