Indications for Replantation and Recommended Techniques
 By Dr. Samuel I. Kratchman
By Dr. Samuel I. Kratchman
“So, you want to pull out my tooth and fix it and put it back in? Are you serious?”
This may be the response from a patient when explaining a replantation treatment plan, to which the reply should be, “For decades, physicians have been transplanting organs from human to human or from animal to human, with the fear of rejection. This is not the case with extraction/replantation because the tooth is being returned to its original socket, therefore minimizing the concern of rejection.”
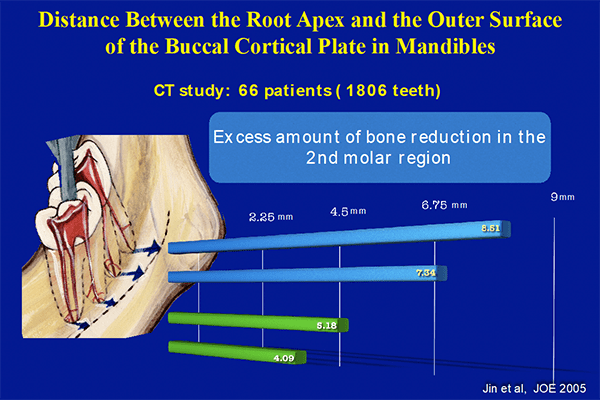
What was once thought of as a procedure of last resort, replantation is a procedure that has been performed successfully for decades, with a success rate just reported in the December 2017 issue of the Journal of Endodontics of 89.1 percent. As endodontists, we should all be competent and skilled at conventional endodontics, nonsurgical retreatment and surgical retreatment, as well as replantation. Of course, conservative retreatment or surgical retreatment should always be considered first when dealing with recurrent endodontic infection, but there are several situations where a retreatment may have been done but a surgical approach would be too difficult, if not impossible, or too risky. For example, mandibular second molars are typically lingually inclined and with the external oblique ridge present, can be covered by approximately 8 mm of bone. In addition, stretching a patient’s lip that far back to retract the soft tissue is often difficult and uncomfortable for the patient.
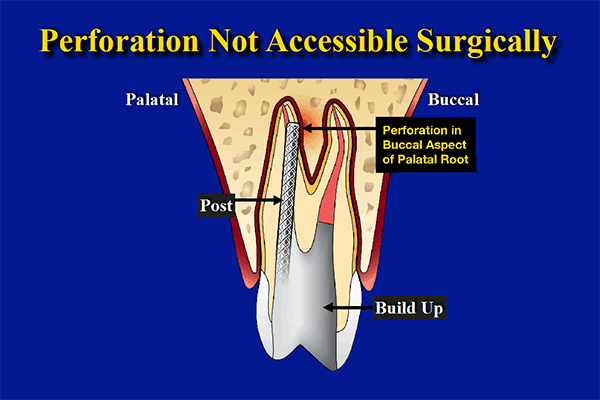
Another indication for replantation is when the tooth is positioned too close to the mandibular canal or mental foramen or completely in the sinus, and surgery could cause irreversible damage or permanent paresthesia. Some cases present with iatrogenic damage to a tooth where a post may perforate in an area that is inaccessible surgically. One would have to remove healthy bone and root in order to approach this perforation site, thereby compromising the crown/root ratio of the tooth, whereas if the tooth was extracted and the perforation site repaired and then replanted, this would not compromise the tooth.
The recommended technique to extract a tooth treatment planned for replantation is to grab the tooth with forceps on enamel or the crown, at or coronal to the CEJ, and gently luxate buccally and lingually/palatally, as well as slight rotational forces, in order to create an acute inflammatory response in the PDL space, resulting in increased mobility until the tooth can be extracted atraumatically. This cannot be rushed, because the tooth must be removed without fracturing it, and if the crown comes off during extraction, it is recommended to place it back on with temporary cement outside the mouth, before replanting the tooth.
Once the tooth has been extracted atraumatically, the rest of the procedure is easy, because the root end resections and fillings are performed extra-orally while keeping the tooth moist with a solution such as Hanks Balanced Salt Solution (Lonza, Inc.; Walkersville, Md.) or Pedialyte (Abbott Pharm; Abbott Park, Ill.). These solutions will maintain the viability of the PDL for up to 30 minutes, whereas the procedure should take no more than 10-15 minutes extra-orally. Most if not all of the granulation tissue often comes out attached to the tooth. If there is still some tissue left in the socket one can pluck it out with tissue forceps but do not curette the walls of the socket. Extracting a tooth severs the periodontal ligament fibers and the remaining fibers lining the inner walls of the socket are critical for re-attachment of the tooth minimizing ankylosis. Once the tooth is replanted, the buccal and lingual/palatal plates of bone are manually compressed, the patient bites down on gauze for 10-15 minutes while post-operative radiographs are taken and the patient receives post-treatment care instructions; and then the mobility of the replanted tooth is assessed. Only if mobility of +2 or greater exists is it necessary to splint the replanted tooth, and this can be accomplished by either suturing over the occlusal surface of the tooth or using a fiberglass-type rope to splint to an adjacent tooth. The need for splinting occurs in less than 20% of the cases, and unnecessary splinting can actually promote ankylosis (replacement resorption), which is the number one cause of failure for replantation. Spot areas of ankylosis will not cause failure, but it is advisable to allow for physiologic mobility, and if failure occurs it is usually within the first year after replantation.
Many articles have been written about replantation from the 1960s to present day, and a systematic review of these articles published in the December 2017 JOE states a success rate of 89.1 percent, along with the comments that replantations are more cost-effective than a single tooth implant and if a replantation is not successful, there is always the alternative of an implant.
Dr. Samuel I. Kratchman is a clinical associate professor of endodontics at the University of Pennsylvania - Philadelphia and maintains three private practices limited to endodontics in Exton, West Chester and Paoli. He can be reached at (610) 524-1610.
Works Cited
- Mainkar, Anshul. A Systematic Review of the Survival of Teeth Intentionally Replanted with a Modern Technique and Cost-effectiveness Compared with Single-tooth Implants. J Endod 2017; 43:1963-8.
- Kim S, Kratchman S. Microsurgery in Endodontics. Wiley Blackwell Publishing.
- Gomez SM, Lallier T. Pedialyte Promotes Periodontal Ligament Cell Survival and Motility. J Endod 2013;39:202-7.
- Kawanami M, Sugaya T, Gama H. Periodontal Healing After Replantation of Intentionally Rotated Teeth with Healthy and Denuded Root Surfaces. Dental Trauma 2001;17:127-33.
