Dental Implants Fail at a Rate 10 Times That of Natural Teeth in Patients with Treated Chronic Periodontitis: Study
 By Scott Froum, D.D.S.
By Scott Froum, D.D.S.
This article originally appeared in Perio-Implant Advisory in April 2021.
Abstract
Dental implants are a commonly used treatment to replace both existing and missing teeth. The long-term survival rate of dental implants has been well-documented in the literature. Long-term retention of teeth in patients with moderate to advanced bone loss, who are treated with periodontal therapy and enrolled in periodontal maintenance programs, yields similar-to-higher long-term success rates.
A recent study comparing the retention rates between dental implants and natural teeth over 10 or more years in patients with a history of chronic periodontal disease found that dental implants were lost at a rate of 10 times that of natural teeth lost due to periodontal disease. With the increasing popularity of full-mouth extractions and replacement with implant-supported prostheses in lieu of teeth-saving periodontal therapy, case selection must be considered prior to implant treatment.
The long-term survival rate of dental implants has been well-documented in the literature1 and is a treatment method widely implemented in general dental offices. Similarly, retention of periodontally treated teeth with moderate to advanced bone loss has similar-to-higher long-term success rates.2 Even natural teeth suffering from advanced bone loss with guarded to poor prognoses treated with initial, surgical, and supportive therapy have high long-term success rates in the literature.3,4 The literature has also shown that patients who adhere to strict hygiene appointments combined with diligent home care can prevent the progression of periodontal disease and maintain their teeth over a long period of time.5
Analyzing the Retrospective Study
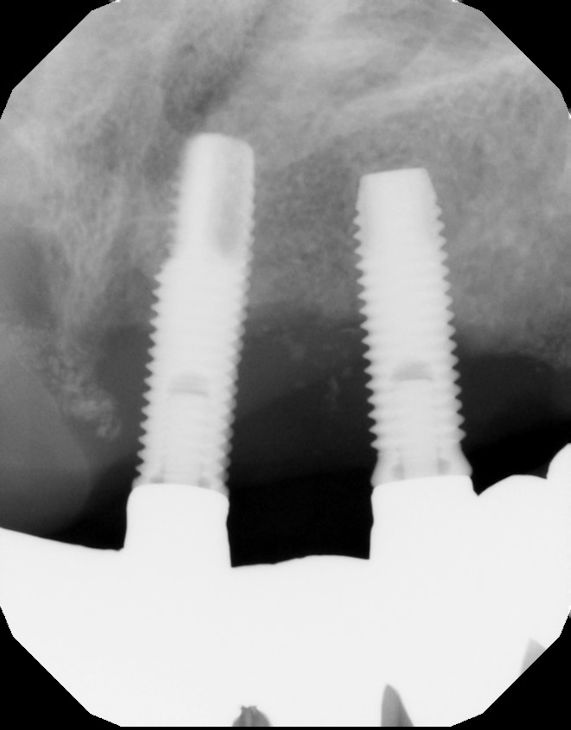
A recent retrospective study with a 10-year follow-up evaluated the long-term survival rates of natural teeth versus dental implants in 58 patients who were treated for chronic periodontal disease and then enrolled in periodontal maintenance programs.6 The study found that over 10 years, overall natural tooth loss (due to caries, endodontic reasons, and/or periodontal reasons) was .07 teeth per patient per year and .04 teeth per patient per year for periodontal reasons.
On the other hand, dental implant loss was 10 times higher, at .4 implants lost per patient per year. Ninety percent of the periodontally compromised teeth treated with active periodontal therapy (i.e., scaling/root planing, surgery, periodontal maintenance) survived over the 10-year period of the study. In addition, teeth designated with questionable prognoses at the baseline decreased by 1.9%, while teeth assigned with good prognoses increased by 3.6%. Overall implant survival in this study population was 90%, with 100% of implants surviving up to five years and then failing at a rate of 10.08% in the six- to 10-year range.
The results of this study agree with other studies suggesting that patients with a history of periodontal disease are more susceptible to implant failure over a prolonged period in function possibly due to bacterial dysbiosis mixed with increases in cytokine production, such as interleukin-1, interleukin-6, tumor necrosis factor alpha and beta. This pathogenic combination can lead to multiple episodes of peri-implantitis over time with potential implant failure.7
Another interesting finding in the study was that over the 10-year follow-up period, implants with a probing depth of six or greater and bone loss of 50% or greater increased 13.5% and 3.1%, respectively, while natural teeth decreased 8% and 10.7%, respectively. This would suggest that tooth prognosis increased over the study period, while implant prognosis decreased. Additionally, patients with probing depths of five or greater and/or full-mouth bleeding scores 25% or greater were at a significant increased risk for peri-implant disease, stressing the importance of controlling periodontal disease in patients who are candidates for implant therapy.8
The authors in this study state: It is generally believed that teeth with unfavorable prognosis should not be treated periodontally because the prognosis of complex therapy may not match the high levels of success of implant treatment. The literature does not support this belief and has indicated that periodontal treatment combined with maintenance therapy of compromised teeth offers high levels of success.9
Historically it was thought that in a patient with periodontal disease, once teeth were removed and implant therapy initiated, the pathogens that caused periodontal tooth loss would be eliminated and therefore not affect the dental implant.10 More recent literature has suggested that this is inaccurate, and patients with either chronic or aggressive periodontal disease may suffer from more biological complications with implant therapy.11
A landmark paper just released that evaluates the difficulty in removing periodontal pathogens from the mouth states: The repopulation of treated periodontal pockets by microbial pathogens may also come from several oral reservoirs, including epithelium and lamina propria of the pocket wall and epithelium of the buccal mucosa, dorsum of the tongue, tonsillar crypts, and saliva.12
One implication of this article would be that once periodontally compromised teeth are extracted, dental implant surfaces can become colonized with potentially disease-causing periodontal pathogens without adequate biofilm control in the overall oral environment. This would apply even in full-mouth extraction cases with immediate or delayed implant therapy.
Deciding on Treatment
In conclusion, when deciding between saving the natural dentition and extracting and placing implants, there are many factors to consider. In addition to long-term success rates, the practitioner and the patient need to evaluate the long-term economic impact the patient will have to endure. With the universal adoption of full-mouth extractions and subsequent treatment with complete arch solutions supported by implants, the drive to extract teeth that can be salvaged with periodontal treatment has increased. Both dental implants and periodontal therapy to save natural teeth have high initial success rates; however, natural teeth often demonstrate fewer complications over time and have less of a financial impact when correction is needed.13
References
- Howe MS, Keys W, Richards D. Long-term (10-year) dental implant survival: a systematic review and sensitivity meta-analysis. J Dent. 2019;84:9-21. doi:10.1016/j.jdent.2019.03.008
- Levin L, Halperin-Sternfeld M. Tooth preservation or implant placement: a systematic review of long-term tooth and implant survival rates. J Am Dent Assoc. 2013;144(10):1119-1133. doi:10.14219/jada.archive.2013.0030
- Setzer F, Syngcuk K. Preserving the natural tooth versus extraction and implant placement: an evidence-based approach. In: Rosen E, Nemcovsky CE, Tsesis I, eds. Evidence-Based Decision Making in Dentistry. Springer; 2017:73-95. doi:10.1007/978-3-319-45733-8_6
- Axelsson P, Lindhe J, Nyström B. On the prevention of caries and periodontal disease. J Clin Periodontol. 1991;18(3):182-189. doi:10.1111/j.1600-051x.1991.tb01131.x
- Hirschfeld L, Wasserman B. A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 1978;49(5):225-237. doi:10.1902/jop.1978.49.5.225
- Guarnieri R, Di Nardo D, Di Giorgio G, Miccoli G, Testarelli L. Longevity of teeth and dental implants in patients treated for chronic periodontitis following periodontal maintenance therapy in a private specialist practice: a retrospective study with a 10-year follow-up. Int J Periodontics Restorative Dent. 2021;41(1):89-98. doi:10.11607/prd.4674
- Karoussis IK, Salvi GE, Heitz-Mayfield LJA, Brägger U, Hämmerle CHF, Lang NP. Long-term implant prognosis in patients with and without a history of chronic periodontitis: a 10-year prospective cohort study of the ITI Dental Implant System. Clin Oral Implants Res. 2003;14(3):329-339. doi:10.1034/j.1600-0501.000.00934.x
- Gay IC, Tran DT, Weltman R, et al. Role of supportive maintenance therapy on implant survival: a university‐based 17 years retrospective analysis. Int J Dent Hyg. 2016;14(4):267-271. doi:10.1111/idh.12188
- Trombelli L, Franceschetti G, Farina R. Effect of professional mechanical plaque removal performed on a long‐term, routine basis in the secondary prevention of periodontitis: a systematic review. J Clin Periodontol. 2015;42(Suppl 16):S221-S236. doi:10.1111/jcpe.12339
- Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res. 2007;18(6):669-679. doi:10.1111/j.1600-0501.2007.01406.x
- Roccuzzo M, Bonino F, Aglietta M, Dalmasso P. Ten‐year results of a three arms prospective cohort study on implants in periodontally compromised patients. Part 2: clinical results. Clin Oral Implants Res. 2012;23(4):389-395. doi:10.1111/j.1600-0501.2011.02309.x
- Cobb CM, Sottosanti JS. A re‐evaluation of scaling and root planing. J Periodontol. 2021. Published online: March 4, 2021. doi:10.1002/JPER.20-0839
- Donos N, Laurell L, Mardas N. Hierarchical decisions on teeth vs. implants in the periodontitis‐susceptible patient: the modern dilemma. Periodontol 2000. 2012;59(1):89-110. doi:10.1111/j.1600-0757.2011.00433.x
Scott Froum, D.D.S., a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of the American Board of Periodontology, is a clinical associate professor at SUNY Stony Brook School of Dental Medicine in the department of periodontology. He serves on the board of editorial consultants for the Academy of Osseointegration’s Academy News. Contact him through his website at drscottfroum.com or (212) 751-8530.